Vaccination is a critical child survival intervention. Immunization at birth is critical to prevent a child from deadly diseases and is helpful in reducing disease burden [1]. The national policy on immunization recommends vaccinating children against preventable diseases like tuberculosis, polio, hepatitis B virus (HPV) during their life course which begins at birth [2-3]. While BCG vaccination to control tuberculosis mainly started since the early 1960s and oral polio vaccine (OPV) was introduced into India’s routine immunization since the 1980s, the inclusion of Hepatitis B and vitamin K prophylaxis into India’s routine new-born care services is relatively recent [2,4]. Examination of the coverage of these vaccines is critical. Vitamin K Deficiency Bleeding which is a significant threat to neonates can also be prevented almost entirely by Vitamin K1 administration soon after birth [5]. India also carries a notable burden of chronic HBV infections globally hence every infant must receive the Hepatitis B birth dose for complete immunisation against this infection [2]. Timely delivery of birth doses of such critical vaccines is also seen as an indicator of the overall performance of immunization programs [1].
The current policy brief examines coverage of birth doses of 4 vaccines mandated by current policy. The brief uses data between FY18 to FY20 from the Health Management Information System (HMIS) which is a source that monitors critical health indicators at state level on a monthly basis.
Coverage of birth vaccination
In Maharashtra, live births peak in the months of September–November and thereafter there is a dip that prolongs from January till June. Similarly, the 4 vaccines that are mandated at birth i.e., Bacille Calmette-Guerin (BCG), Hepatitis B, oral polio (OPV) and Vitamin K1 also have the highest coverage during the same months. The coverage of birth related immunization dips is usually the lowest in the months of February -April. In terms of coverage of birth doses of the 4 vaccines, the largest gap existed for Hepatitis B and vitamin K1 birth doses. The gap between number of births and oral polio vaccine (OPV) was relatively low (Figure 1).
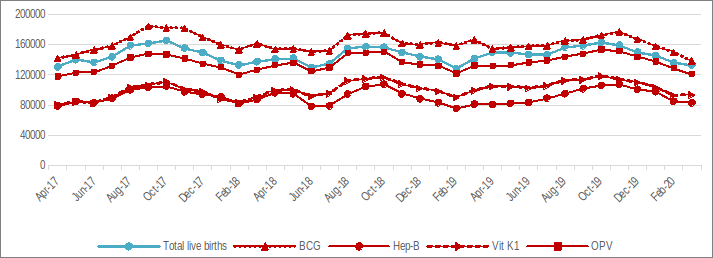
The numbers of Bacille Calmette-Guerin (BCG) exceeded that of children born through FY18-FY20 indicating possibility of over-reporting or duplication however this needs further scrutiny.
What factors affect birth vaccination coverage?
According to HMIS data, a considerable proportion of newborns were not covered by vitamin K1 prophylaxis and Hepatitis -B birth doses. However, data indicates the timelines for the birth doses of these vaccines is likely to be important as the earlier the deadline to administer the dose, the higher the chances of missing the birth dose of the given vaccine. As per immunization guidelines, the birth dose of BCG could be administered to the infant latest by the first year of life whereas OPV could be administered within the first 15 days of life. However, Vitamin K1 and Hepatitis B birth doses need to be given within 24 hours of birth [3,5]. Moreover, both vaccines are required to be injected intramuscularly. Hence, home deliveries can be hindrance to improving coverage of birth doses of these 2 vaccines.
Poor coverage of Vitamin K1 has also been attributed to supply side shortcomings and poor awareness of health workers [6]. While there is a policy that mandates administration of injection Vitamin K Prophylaxis at birth, the national immunization schedule has not included this vaccine which indicates the need to sensitize health care workers on its importance [3,5].
Factors like maternal education and antenatal care (ANC) utilization also determine an infant’s hepatitis B immunisation status [2]. Poor stock management, incomplete recording and poor knowledge amongst health functionaries about vaccination schedule have resulted in the low uptake of hepatitis B birth dose. Fear of wastage of hepatitis B vaccine in 10 dose vial in peripheral facilities with few births was another concern. While the open vial policy has helped to reduce wastage of vaccines , further monitoring may be needed [7-8].
Policy Implications & Recommendations
HMIS data shows that a significant proportion of infants did not receive doses of vaccines that had to be administered shortly after delivery―Vitamin K1 and Hepatitis B. However, NFHS 5 reported that only 5 of the 36 districts in the state have an institutional delivery rate below 90 percent [9]. This also highlights that even if babies are born in health facilities, there is a high likelihood that they won’t receive the birth doses of the two vaccines. Hence, it is critical not only to improve rates of institutional births in regions that are still reporting notable rates of home deliveries but also to improve outreach and delivery of immunization services. Sub-centers and primary health centers should receive an adequate supply of vaccines including Vitamin K prophylaxis. State health officials must conduct periodic inspections to ensure the availability of logistics in accordance with policy [5].
The District Health Department also needs to sensitize healthcare workers like auxiliary nurse midwives (ANM) and accredited social health activists (ASHA) about the importance of providing all birth doses of vaccines like the Hepatitis B and vitamin K1.
All pregnant women should be reminded of the birth vaccines that the newborn has to receive during home visits in the last trimester as well as 4th antenatal care checkup. As per the Home Based Newborn Care guideline10, ASHAs should examine the newborn within six hours of birth. The visit could be used to advise mothers about the birth vaccines or accompany mothers so that they receive birth doses of vaccines.
References
- Gera, R., Kapoor, N., Haldar, P., Gupta, S., Parashar, R., Tomar, S. S., … & Taneja, G. (2019). Implementation of “health systems approach” to improve vaccination at birth in institutional deliveries at public health facilities; experience from six states of India. Journal of family medicine and primary care, 8(5), 1630.
- Khan, J., Shil, A., & Mohanty, S. K. (2019). Hepatitis B vaccination coverage across India: exploring the spatial heterogeneity and contextual determinants. BMC Public Health, 19(1), 1-14.
- Ministry of Health and Family Welfare. (2018). National Immunization Schedule. National Health Mission.
- Lahariya, C. (2014). A brief history of vaccines & vaccination in India. The Indian journal of medical research, 139(4), 491.
- Ministry of Health & Family Welfare. (2014). Injection of Vitamin K Prophylaxis at Birth. Retrieved from https://nhm.gov.in/images/pdf/programmes/child-health/guidelines/Vitamin_K_Operational_Guidelines.pdf
- Bora, K. (2021). Gaps in the coverage of vitamin K1 prophylaxis among newborns in India: insights from secondary analysis of data from the Health Management Information System. Public Health Nutrition, 24(17), 5589-5597.
- Lahariya, C., Subramanya, B. P., & Sosler, S. (2013). An assessment of hepatitis B vaccine introduction in India: Lessons for roll out and scale up of new vaccines in immunization programs. Indian journal of public health, 57(1), 8.
- UNICEF. (2021). A report on the assessment of Open Vial Policy Implementation in India. National Cold Chain and Vaccine Management Resource Centre.
- Ministry of Health and Family Welfare. (n.d.). Women 15-49 year old who delivered in a health facility, Maharashtra, NFHS5 2019-2021 By District. Retrieved from https://healthnutritionindia.in/dashboard/4/2/75
- Ministry of Health and Family Welfare. (2014). Home based newborn care operational guidelines. Retrieved from https://nhsrcindia.org/sites/default/files/2021-03/Revised%20HBNC%20Operational%20Guidelines%202014%20English.pdf
We acknowledge the support of the National Health Mission, CTARA-IIT Bombay, and the GISE Hub, IIT Bombay.
Authors
Marian Abraham, Prof. Sarthak Gaurav, Animesh Nautiyal
Marian Abraham is a Senior Research Analyst at the Koita Centre For Digital Health, IIT Bombay.
Prof. Sarthak Gaurav is an Associate Professor at Shailesh J. Mehta School of Management, IIT Bombay.
Animesh Nautiyal is a Project Research Assistant at Shailesh J. Mehta School of Management, IIT Bombay.
