Envenoming and deaths due to snakebites is a neglected disease that largely affects the marginalized in many tropical countries. Severe snakebite envenoming can cause severe tissue destruction resulting in permanent disability, cause kidney failure, respiratory failure or induce bleeding disorders that lead to hemorrhage that is fatal [1]. The morbidity and mortality associated with snakebite envenoming can be prevented through timely medical interventions such as the use of snake anti-venoms [2-3]. Recognizing the need to prioritize action, the WHO has set a target to reduce disability and mortality from snakebites to 50% by 2030 [1]. Globally, India accounts for most of the snakebite envenoming and mortality burden. At 81,000 cases per year, India had the highest snakebite envenomings annually than any other country. India also accounts for more than half of the 20,000 annual snakebite deaths that occur globally [4]. Maharashtra has the highest prevalence of snakebite envenoming in the country [5]. Identifying the most vulnerable populations and regions at risk would be key to managing the problem.
A detailed evaluation of spatial-temporal patterns of snakebite envenoming and mortality at the state level can be vital to support local health systems, planning, and distribution of resources in high-burden regions. The current policy brief uses Health Management Information System (HMIS) data from FY18-FY20 in Maharashtra for this purpose.
Seasonality in the prevalence of snake envenoming?
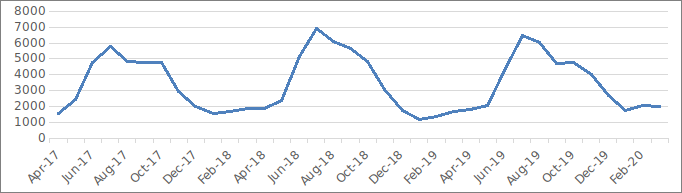
The increasing incidence of snakebites poses a significant public health challenge. Maharashtra recorded a 9.8% rise in snakebite emergency cases within a short period ― cases went up from 38,936 in 2017-18 to 42,756 in 2019-20. The occurrence of snakebite emergencies has a strong seasonal pattern. Snakebite incidence in the state appears to be driven by agro-climatic factors — cases peak during the first two months of the monsoon i.e., July and August, and thereafter decline steadily with a significant dip in the months of January-February (Figure 1). The risk of snakebite envenoming appears to be the highest during the first two months of monsoon also when paddy and major legume crops are cultivated during the Kharif farming season [6]. Reliance on non-mechanized and barefoot techniques places agrarian workers at a high risk of snakebites [7]. Monitoring is required to manage emergencies during peak periods.
Snakebite incidents during the kharif cropping season have been attributed to krait even though cobra and Russell’s viper bites are often reported from the districts in Maharashtra where farming is the main occupation [9].
Seasonal variation in mortality due to animal bites/sting?
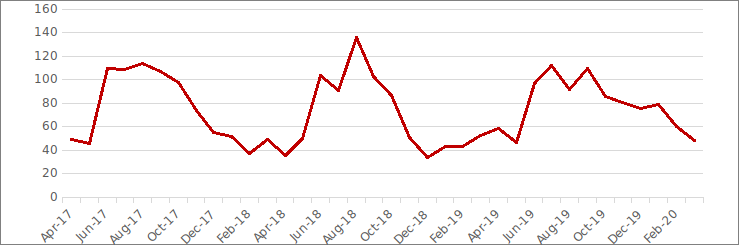
In Maharashtra, adolescent/adult deaths due to animal bites and stings including snakebites escalate between the months of June and September. The peak in mortality due to animal bites coincides with a peak in snakebite emergencies which indicates the possibility that many of these deaths occurred due to snakebite envenoming (Figure 1-2). Complications of snakebite develop rapidly and irreversibly hence medical intervention has to be prompt and appropriate. Adequate clinical management of snakebite envenoming implies the use of appropriate first aid methods, timely referral and presentation to health center, and appropriate diagnosis and treatment [2]. Local administration must monitor the situation during the months of peak incidence to deal with the evident gap in the management of snakebite envenoming to prevent mortality.
Districts with the highest snakebite cases also have high mortality?
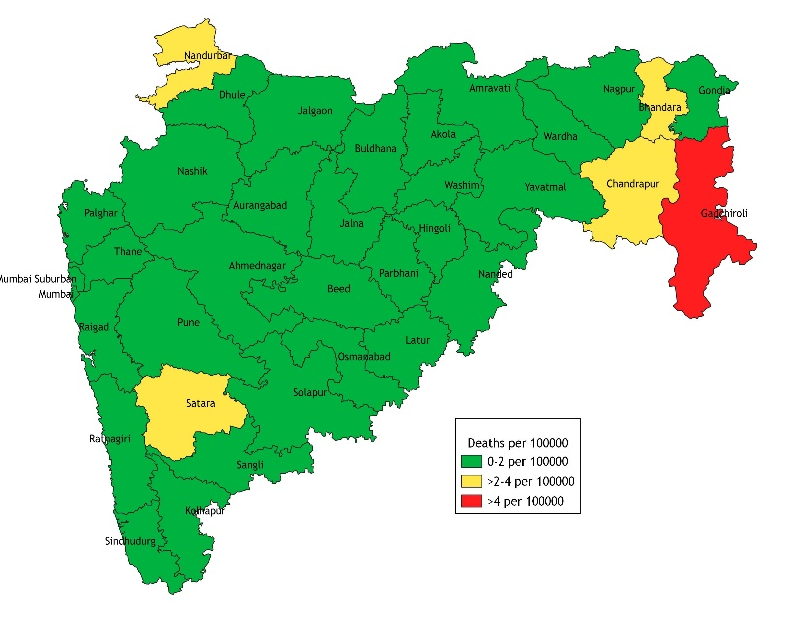
Identifying regions that constitute the highest burden of snakebite envenoming and mortality is critical to prioritize action. In 2019-20, the highest rate of snakebites was reported from 3 districts of Maharashtra―Sindhudurg, Ratnagiri and Palghar (Figure 3).
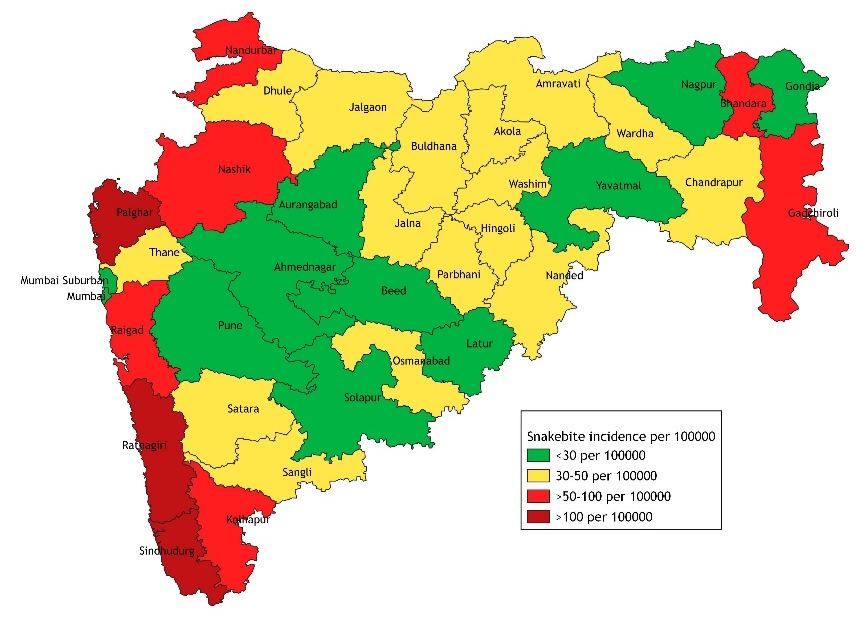
Gadchiroli would be a focus district given that it reported a high rate of snakebite emergencies as well as one of the highest burdens of adult/adolescent mortality due to animal bites and stings in the state (Figure 4). This could be an indication of the gross gap in capacities in managing snakebite envenoming. Early treatment interventions may save the lives of many associated with agriculture or living in rural settings [5].
Policy Implications
The identification of high-burden districts and periods of peak and low incidence of snakebite emergencies and mortality can aid health system decision-making. It can help in identifying the periods where local administration can monitor the incidence and also prioritizing locations to establish specialized centers for snakebite management. Local administration could maintain adequate stocks of vials of anti-venom of medically important snake species in primary health centers and community hospitals during peak periods. In high-priority regions, the administration can ensure the availability of equipment that is critical in recovery and survival.
Recommendations
Snakebite envenoming is a life-threatening hazard but it can be treated and even prevented. It is critical that local health systems are strengthened to adequately manage and control this hazard. Better allocation of resources including the availability of life-saving equipment, diagnostic test kits, and distribution of snake anti-venom (ASV) vials in primary health centers and hospitals as per guidelines is vital. Districts with high snakebite envenoming burden must be monitored by the Health Department.
A genuine concern is that healthcare workers at the referral health facility are possibly not complying with the standard treatment protocols, or that they lack full knowledge about the ASV dose or its administration [8]. Health department district training centers can conduct sensitization and training of healthcare workers on the assessment of envenomation and management of snakebites as per the set protocol and national guidelines [2,3].
Cases of snakebite envenoming would also reduce with an improvement in community awareness about the risk of snakebites, myths about traditional healing, symptoms of snakebites, appropriate first aid methods, and the treatment available in public health facilities. They should be encouraged to seek facility care for appropriate case management.
References
- World Health Organization. (2019). Snakebite envenoming: a strategy for prevention and control. Retrieved from https://www.who.int/publications/i/item/9789241515641
- World Health Organization. (2016). Guidelines for the management of snakebites. Retrieved from https://www.who.int/publications/i/item/9789290225300
- Ministry of Health & Family Welfare. (2015). Standard Treatment Guidelines. Management of Snakebite. Quick Reference Guide. Government of India.
- Kasturiratne, A., Wickremasinghe, A. R., de Silva, N., Gunawardena, N. K., Pathmeswaran, A., Premaratna, R., … & de Silva, H. J. (2008). The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS medicine, 5(11), e218.
- Salve, P. S., Vatavati, S., & Hallad, J. (2020). Clustering the envenoming of snakebite in India: The district level analysis using Health Management Information System data. Clinical epidemiology and global health, 8(3), 733-738.
- DESAGRI. (n.d.). Crop calendar of major crops. Directorate of Economics and Statistics, Department of Agriculture and Farmers Welfare. Ministry of Agriculture and Farmers Welfare. Retrieved from: https://desagri.gov.in/document-report/4-crop-calendar-of-major-crops/
- World Health Organisation. (2021). Snakebite envenoming Factsheets. Retrieved from: https://www.who.int/news-room/fact-sheets/detail/snakebite-envenoming
- Bawaskar, H. S., Bawaskar, P. H., Punde, D. P., Inamdar, M. K., Dongare, R. B., & Bhoite, R. R. (2008). Profile of snakebite envenoming in rural Maharashtra, India. JAPI, 56, 88-95.
- Gajbhiye, R., Khan, S., Kokate, P., Mashal, I., Kharat, S., Bodade, S., … & Mahale, S. (2019). Incidence & management practices of snakebite: A retrospective study at Sub-District Hospital, Dahanu, Maharashtra, India. The Indian Journal of Medical Research, 150(4), 412.
We acknowledge the support of the National Health Mission, CTARA-IIT Bombay, and the GISE Hub, IIT Bombay.
Authors
Marian Abraham, Prof. Sarthak Gaurav
Marian Abraham is a Senior Research Analyst at the Koita Centre For Digital Health, IIT Bombay.
Prof. Sarthak Gaurav is an Associate Professor at Shailesh J. Mehta School of Management, IIT Bombay.
