Preterm births are babies that are born before 37 completed weeks of gestation.1 Preterm birth-related complications accounted for 16% of all deaths among children under the age of 5 years and 35% of deaths among newborn babies in 2018 globally.2 Preterm infants who survive face an elevated risk of neurodevelopmental impairments and respiratory complications.1 There is also evidence that compared to term babies, preterm babies are at a significantly higher risk of becoming underweight and stunted in the first two years of life.3 One of the targets of the third Sustainable Development Goal is to reduce the mortality of children younger than 5 years and prevention of preterm births and adequate care of preterm infants is critical to ensure that progress is made toward delivery of this target.4 Achieving this goal would require targeted action in regions that report the highest burden of preterm births.
The Health Management Information System (HMIS) is the only source that monitors critical health indicators below the state level every month. In the current policy brief, the HMIS data for the financial years 2017-18 to 2019-20 is examined to understand the patterns of preterm births in Odisha.
Prevalence of Preterm births in Odisha
Odisha consistently reported high preterm birth rates between FY18 to FY20. According to HMIS data, the preterm birth rate was 56 per 1000 live births in 2017-18 which increased to 60 in 2018-19 but again marginally declined to 59 in 2019-20.
Districts with the highest preterm birth rates in Odisha?
It is important to identify districts of high and low preterm birth incidence to help policymakers make informed decisions and take action. District-wise data shows that 7 districts i.e. Nabarangapur, Rayagada, Kendujhar, Sundargarh, Koraput, Kandhamal, and Boudh consistently featured among the 10 highest preterm incidence districts during FY-18 to FY-20. It is worth noting that 6 of these 7 districts are known to have a significant population of Scheduled Tribes.5
Source: HMIS
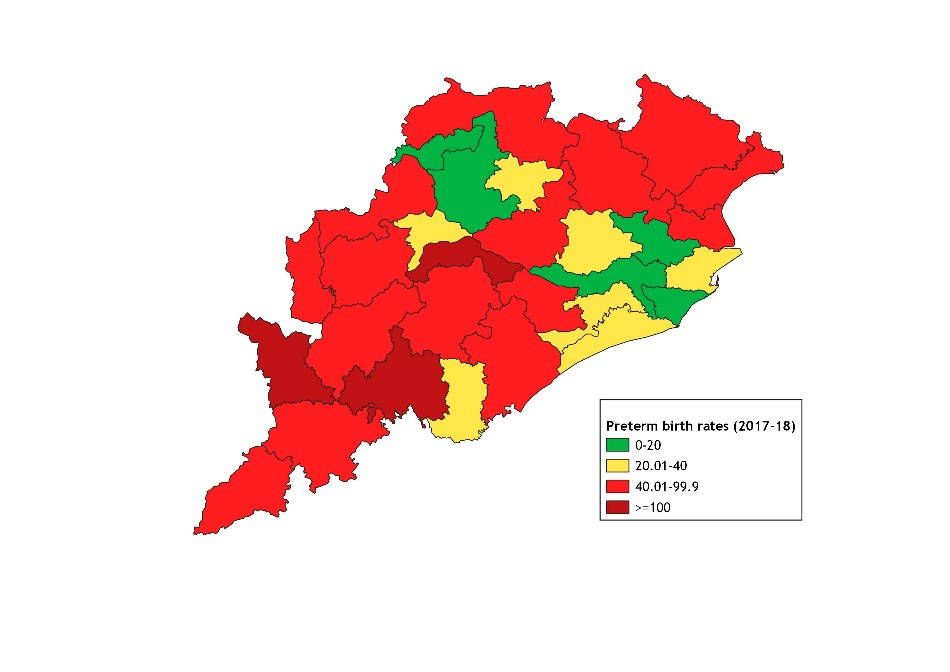
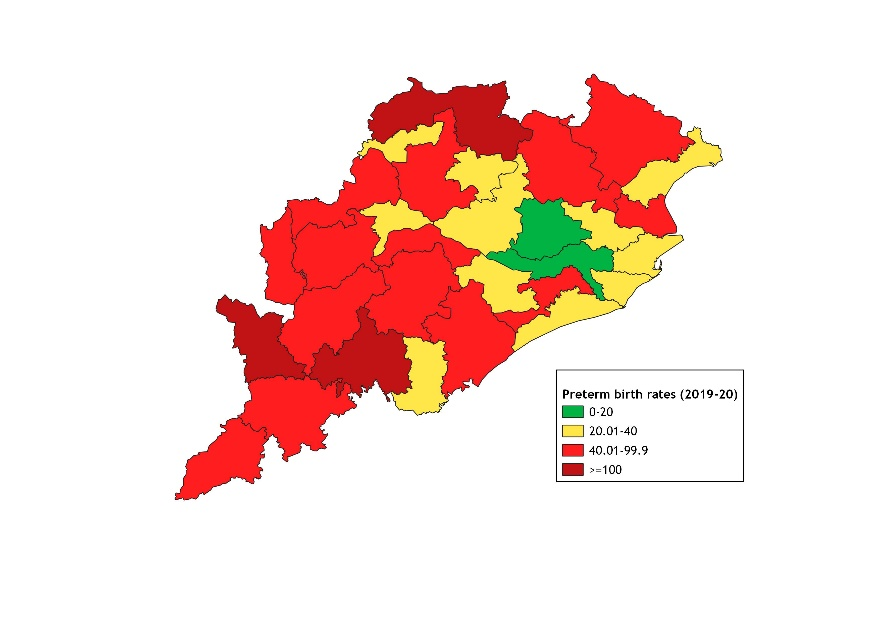
Figure 1 & 2 presents color-coded maps of preterm birth rates (PTR) during 2017-18 and 2019-20. The most prominent clusters with high incidence were located in the southern part of the state. Most districts that reported high PTR in 2019-20 also reported a high PTR in 2017-18 however there have been visible changes in a few districts. The situation in Sambalpur, Sundargarh, Nabarangpur, Khordha and Bhadrak needs to be monitored closely as there has been a significant spike (>20 percentage point increase) in preterm birth rates within a short period between FY18 and FY20. In contrast, despite significantly reducing preterm birth rates since FY18, Boudh, Balangir, Kendujhar, and Kalahandi districts still have high rates of preterm births.
Source: HMIS
Priority blocks for targeted action
It is instructive to identify which blocks within the priority districts have the highest preterm birth incidence and hence action should be prioritized. 15 blocks with the highest incidence in the state were largely located in districts with high or very high incidence of preterm births. However, the preterm birth rates in these blocks were unusually high and may require further scrutiny (Table 1).
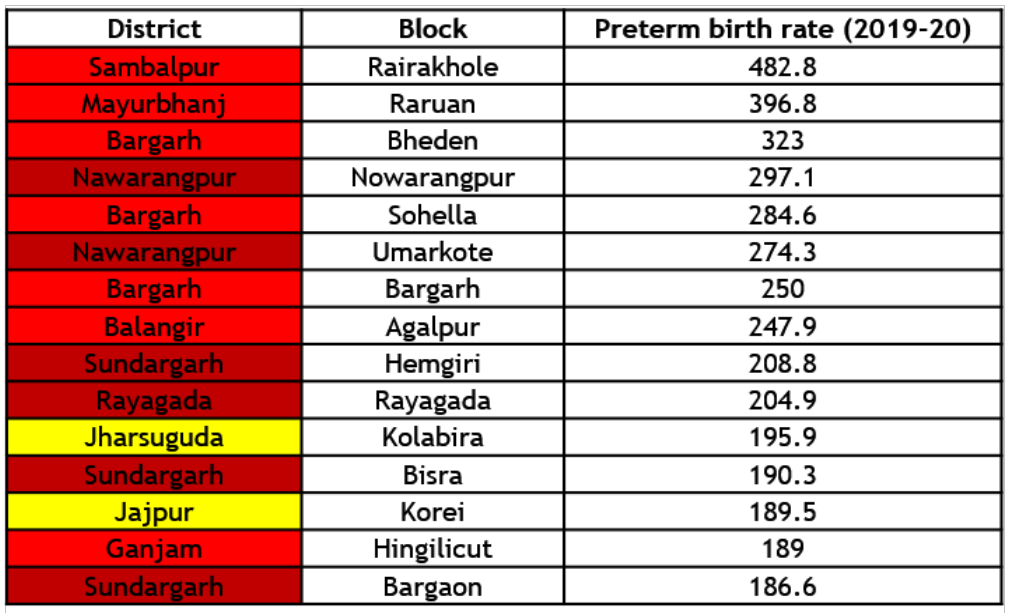
The color-coded map highlights the blocks that reported high (red) and very high (dark red) rates of preterm births in 2019-20 (Figure 3). 50 blocks with very high rates belonged to 18 districts spread across the state. While 12 of these blocks were located in the 3 districts (Rayagada, Nabarangpur and Sundargarh) that reported very high preterm birth rates, a prominent cluster of blocks with very high rates were also located in districts with low and moderate incidence. Cuttack which reported a low preterm birth rate also reported that 3 of its blocks had very high rates in 2019-20. At the state level, curtailing preterm births in such districts could be a low-hanging fruit.
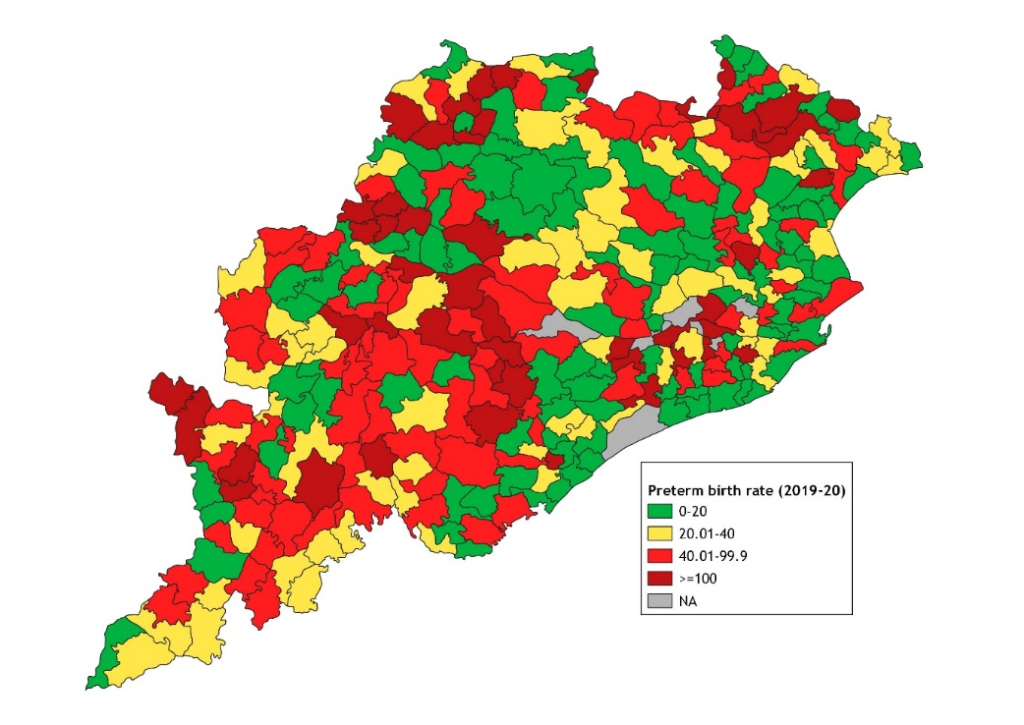
Fig 3. Preterm birth rates (per 1000 live births) across blocks of Odisha, FY20
Source: HMIS
Reducing & Managing Preterm Births: Key Action Points
Odisha is a state with high preterm birth incidence where few districts and blocks have reported preterm birth rates that exceed 100 per 1000 live births. The identification of such districts and blocks with the highest incidence in the state can aid local administrators in the micro-planning of health and nutrition interventions in these areas.
Health system strengthening is fundamentally crucial in regions with high preterm birth rates. This includes ensuring the availability of quality healthcare facilities and trained personnel as per caseload and existing norms. Medical officers and ANMs also need to be given adequate training for the appropriate administration of antenatal corticosteroids as per guidelines.6 Further, the Public Health Department should additionally conduct refresher training so that frontline healthcare workers like ASHAs are adequately able to identify high-risk mothers and assess signs of preterm labor.
In the Indian context, maternal anemia, pregnancy-induced hypertension, prior history of preterm labor, low maternal height, and low birth spacing have been recognized as risk factors for preterm births.7-9 Obstetric factors, such as minimal antenatal care, delivery complications, history of previous cesarean delivery, and delivery at private health facilities are also associated with an increased risk of PTB.7 Hence, antenatal and delivery care play a critical role in the prevention and management of preterm births.9
Ensuring more pregnant women receive their routine antenatal care (ANC) visits and investigations including ultrasonography promptly is important. To ensure that pregnant women report early to health facilities, ANM/ASHAs must provide counselling to pregnant women and their families about the first signs of preterm labor, symptoms of pregnancy complications, birth preparedness, and the need to opt for institutional delivery. Timely referral of women in preterm labor as per guidelines to nearest facilities that provide caesarean section, special care newborn units, and preferably also Kangaroo Mother Care units is vital.6,10
Post-discharge, periodic home visits by ASHAs to monitor health and support breastfeeding of preterm newborns as per the Home Based New Born Care schedule would be critical to preventing adverse outcomes related to preterm births.11
References
- Goldenberg, R. L., Culhane, J. F., Iams, J. D., & Romero, R. (2008). Epidemiology and causes of preterm birth. The lancet, 371(9606), 75-84.
- UNICEF. (2019). Levels & trends in child mortality- Report 2019: Estimates/developed by the UN Inter-Agency Group for Child Mortality Estimation.
- Santos, I. S., Matijasevich, A., Domingues, M. R., Barros, A. J., Victora, C. G., & Barros, F. C. (2009). Late preterm birth is a risk factor for growth faltering in early childhood: a cohort study. BMC Pediatrics, 9, 1-8.
- World Bank. (n.d.). Sustainable Development Goals and Targets.
- Government of India. (2011). Odisha district wise map-ST percentage. Retrieved from: https://www.censusgis.org/india/
- MoHFW. (2014). Use of Antenatal Corticosteroids in Preterm Labour. Operational Guidelines. National Health Mission. Ministry of Health and Family Welfare.
- Jana, A., Banerjee, K., & Khan, P. K. (2022). Early arrivals: association of maternal obstetric factors with preterm births and their survival in India. Public Health, 211, 37-46.
- Kumari, S., Garg, N., Kumar, A., Guru, P. K. I., Ansari, S., Anwar, S., … & Sohail, M. (2019). Maternal and severe anaemia in delivering women is associated with risk of preterm and low birth weight: A cross sectional study from Jharkhand, India. One Health, 8, 100098.
- Sureshbabu, R. P., Aramthottil, P., Anil, N., Sumathy, S., Varughese, S. A., Sreedevi, A., & Sukumaran, S. V. (2021). Risk factors associated with preterm delivery in singleton pregnancy in a tertiary care hospital in south India: a case control study. International Journal of Women’s Health, 369-377.
- MoHFW. (2011). Guidelines for Janani Shishu Suraksha Karyakram. Ministry of Health and Family Welfare.
- MoHFW. (2014). Home-Based Newborn Care. National Health Mission. Ministry of Health and Family Welfare.
We acknowledge the support of the National Health Mission, CTARA-IIT Bombay, and the GISE Hub, IIT Bombay.
Authors
Marian Abraham, Prof. Sarthak Gaurav
Marian Abraham is a Senior Research Analyst at the Koita Centre For Digital Health, IIT Bombay.
Prof. Sarthak Gaurav is an Associate Professor at Shailesh J. Mehta School of Management, IIT Bombay.
