Birth outcomes are critical indicators of community and individual well-being hence high incidence of adverse birth outcomes (such as preterm births and stillbirths) are a major public health concern.1 Preterm births contribute to long-term morbidity and neonatal mortality hence their prevention is strongly advocated.2 However, the prevention of stillbirths, an adverse birth outcome closely linked to preterm births also needs to be emphasized strongly in policy agendas given that the combined number of deaths related to preterm births and stillbirths is significant.3 Data on the distribution of these adverse birth outcomes can be critical for planning maternal healthcare interventions and tracking progress. Studies have observed seasonal variation in the incidence of preterm and stillbirths but there is a notable paucity of such evidence at state and national levels.1,4
The Health Management Information System (HMIS) is the only source that monitors critical health indicators below the state level on a monthly basis. It also covers important outcomes like preterm and stillbirth rates in Maharashtra. Using HMIS data, the policy brief examines whether there is seasonality in preterm and stillbirth rates and review related policy implications. Data prior to the onset of the pandemic was used, i.e. FY 2017-18 to 2019-20.
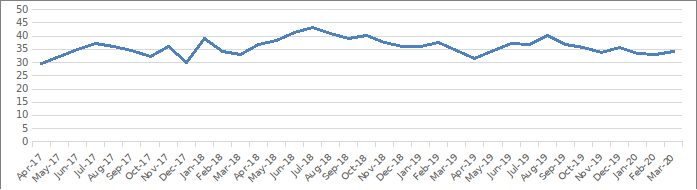
Seasonality in preterm births?
The identification of preventable risk factors for preterm births of major public health importance. It hence may be critical to also review the variation in preterm births. Data from FY 2017-18 to FY 2019-20 does indicate some seasonality in the occurrence of preterm births in Maharashtra. Annually, the highest preterm birth rates were usually observed between July- August. Following this peak, there is a dip in September and a spike in rates again in October. The rates again increase around January-February. Preterm birth rates are usually low between March-April (Figure 1). The spike in preterm birth rates coincides with the monsoon season when the prevalence of infectious diseases is high.5 The period of July-August also corresponds to the Kharif farming season. Preoccupation with hard physical labour for long hours under stressful conditions is likely associated with an increase in preterm birth.2
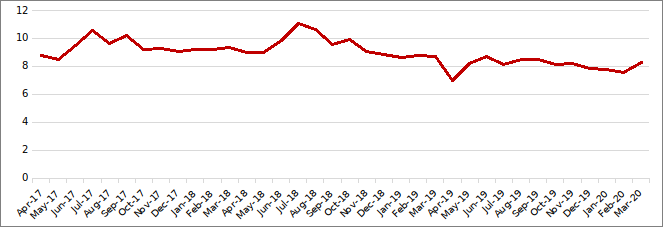
Is there seasonal variation in stillbirths?
While it appears that even stillbirth incidence is influenced by the farming and monsoon seasons, stillbirths showcase a more prominent pattern of seasonality compared to preterm births. This also suggests the presence of potential risk factors associated with the season. Stillbirth rates increase from May and peak usually in July. However post-peak, there is a steady decline in stillbirth rates that continues till April when stillbirth rates are the lowest (Figure 2).
To an extent, the peak of stillbirth rates in July coincides with the first peak (July-August) in preterm birth rates which indicates the possibility of the peaks being related as has also been observed previously.4 Also, the period (May-June) when stillbirth rates start increasing is the hottest. It is known that exposure to high temperatures induces dehydration which has implications for adverse pregnancy outcomes like stillbirths.4
Key Takeaways & Policy Implications
The data indicates that there is some seasonality in the occurrence of adverse birth outcomes, especially stillbirths. The maximum preterm birth rate was usually reported between July-August whereas the stillbirth rates were usually high between June-July. The data also has policy implications. Seasonal patterns would possibly reflect the different etiologies of these adverse birth outcomes. Hence, identifying critical windows of susceptibility would help local administrators determine the potential risk factors that may necessitate programmatic action, plan targeted action for certain groups, or determine the appropriate periods for effective interventions to prevent preterm births and stillbirths. For instance, the regularity of peaks in preterm births or stillbirths can also help local administrators charged with improving obstetric care to plan the dissemination of education messages or maintain stocks of drugs needed to reduce the risk of preterm labour.6
Policy Recommendations
Timely identification of pregnancy complications plays a critical role in preventing and managing adverse birth outcomes. Hence, early registration of pregnancies and conducting the required antenatal visits as per mandate is critical.7 Tracking pregnant women, especially those who were classified as high risk till completion of the term is important to ensure adequate antenatal care and case management. Maintenance of information/records, distribution of maternal and child protection (MCP) cards, and frequent home visits by healthcare workers would be crucial for this purpose.
Healthcare workers must counsel pregnant women and their families on nutrition and care during pregnancy and birth preparedness in addition to informing them about the danger signs of complications, the need to report to a facility at first signs of complications, and the need for institutional delivery. Periodic training and sensitization of healthcare workers to aid in the identification of high-risk pregnancies and also emphasize key messages related to guidelines for the management of these birth outcomes is also essential.6-7
References
- Osei, E., Agbemefle, I., Kye-Duodu, G., & Binka, F. N. (2016). Linear trends and seasonality of births and perinatal outcomes in Upper East Region, Ghana from 2010 to 2014. BMC pregnancy and childbirth, 16(1), 1-9.
- Goldenberg, R. L., Culhane, J. F., Iams, J. D., & Romero, R. (2008). Epidemiology and causes of preterm birth. The lancet, 371(9606), 75-84.
- Lawn, J. E., Gravett, M. G., Nunes, T. M., Rubens, C. E., & Stanton, C. (2010). Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC pregnancy and childbirth, 10(1), 1-22.
- Bernard, R. P., Bhatt, R. V., Potts, D. M., & Rao, A. P. (1978). Seasonality of birth in India. Journal of Biosocial Science, 10(4), 409-421.
- Locks, L. M., Patel, A., Katz, E., Simmons, E., & Hibberd, P. (2021). Seasonal trends and maternal characteristics as predictors of maternal undernutrition and low birthweight in Eastern Maharashtra, India. Maternal & Child Nutrition, 17(2), e13087.
- Ministry of Health and Family Welfare. (2014). Use of Antenatal Corticosteroids in Preterm Labour. Operational Guidelines. National Health Mission
- Ministry of Health and Family Welfare. (2010). Guidelines for Antenatal Care and Skilled Attendance at Birth by ANMs/LHVs/SNs. National Health Mission.
We acknowledge the support of the National Health Mission, CTARA-IIT Bombay, and the GISE Hub, IIT Bombay.
Authors
Marian Abraham & Prof. Sarthak Gaurav
Marian Abraham is a Senior Research Analyst at the Koita Centre For Digital Health, IIT Bombay.
Prof. Sarthak Gaurav is an Associate Professor at Shailesh J. Mehta School of Management, IIT Bombay.
