Soil-transmitted helminth (STH) infections are an important cause of the burden of morbidity globally, affecting an estimated 1.5 billion people worldwide, the majority of which are women of reproductive age (WRA) including pregnant women1. STH infections result in severe blood loss and malabsorption of nutrients2. Pregnant women with intestinal worm infections are at an increased risk of maternal complications and adverse outcomes such as anemia, low birth weight, and perinatal mortality1. Deworming is one of the primary preventive approaches to deal with STH globally and its use does not result in adverse birth outcomes2 instead, studies have observed that antenatal deworming reduces the risk of maternal anemia, childhood anemia and stunting, low birth weight, and neonatal mortality3-5. In recognition of the efficacy and importance of preventive deworming therapy, the WHO recommends administering deworming through anthelminthic drugs like albendazole in pregnant women post the 1st trimester6. In accordance with WHO, the national guidelines on antenatal deworming prescribe a single dose of 400 mg of albendazole after 1st trimester, also recognizing that iron and folic acid tablets are alone inadequate to reduce maternal anemia7. India is also known to be endemic for soil-transmitted helminth infections, though prevalence estimates for pregnant women are lacking3. This makes the implementation of deworming interventions critical.
Examination of deworming coverage is vital to track the progress of implementation, reflect on possible gaps in delivery, and support planning to scale up coverage. The Health Management Information System (HMIS) is the only source that monitors critical health indicators below the state level on a monthly basis.
The policy brief examines data of key ANC services from the financial years prior to the onset of the pandemic i.e. FY 2017-18 to 2019-20. The aim of this policy brief is to facilitate understanding of coverage of an important intervention like antenatal deworming and promote its uptake.
Is there adequate coverage of Albendazole?
According to the national protocol, albendazole is the recommended drug for deworming during pregnancy. The mandate requires a single dose of albendazole to be done after the 1st trimester of pregnancy7. As per HMIS data, this mandate is only moderately met in the state―69.1% of pregnant women who received 4 or more ANC visits in Maharashtra were given one albendazole tablet after the 1st trimester in FY 2019-20. However, this coverage is an improvement from the previous years. In 2017-18, only 49.8% of pregnant women with 4 or more ANC visits were given 1 albendazole tablet after the 1st trimester and this notably increased to 61.2% in 2018-19. It is evident that the state must meet the critical gap in deworming coverage to ensure maternal well-being and prevent adverse pregnancy outcomes.
Does Albendazole coverage match up to other ANC services?
The antenatal care (ANC) package includes different services that must be delivered promptly to pregnant women as per set guidelines. HMIS data between FY18- FY 20 shows that among pregnant women who have received 4 or more ANC check-ups, the coverage of one tablet of albendazole post 1st trimester is the least compared to other ANC services though the coverage gap has been steadily reducing since FY 19 (Figure 1).
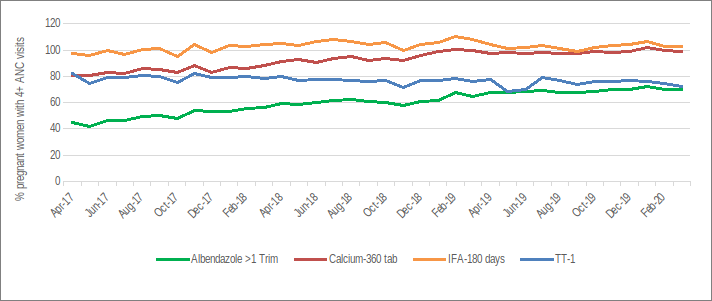
While the universal coverage of iron and folic acid (IFA) tablets for 180 days and 360 calcium tablets raises concerns about over-reporting, it does appear that the implementation of these is efficient. Iron and folic acid tablet distribution and TT injections have been part of the basic ANC package at least since 20108. However, the guidelines that mandate deworming through albendazole tablets and calcium tablets were introduced in the same year i.e. 20147,9 which indicates that the implementation of deworming was not prioritized.
District-level coverage: Where should focus lie?
Coverage patterns of deworming during pregnancy varied throughout the state. In 2019-20, most districts with high coverage (>70% coverage) of albendazole were located in the northern and eastern parts of the state. Nanded, Gondia, Wardha, and Gadchiroli districts consistently reported the highest coverage rates in both 2017-18 and 2019-20 (Figure 2). Most districts with the highest rates of anemia among women of reproductive age as per NFHS -510 also reported the highest deworming coverage. This is evident given that deworming is emphasized as one of the primary interventions to reduce maternal anemia7,11.
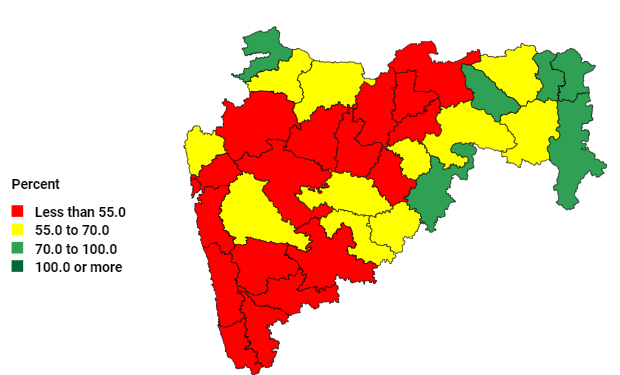
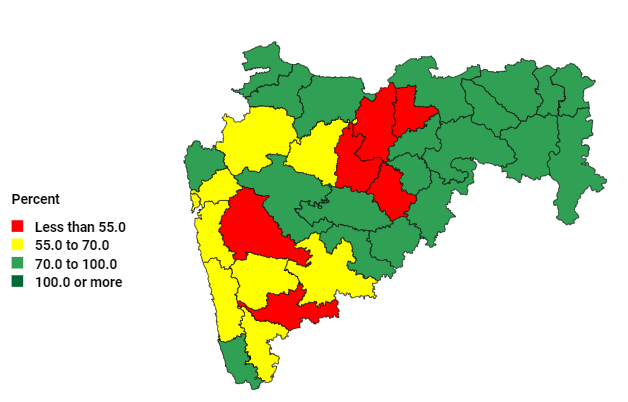
HMIS data also shows that Maharashtra would have to prioritize action in the cluster of districts with the lowest coverage largely located in central Maharashtra―Akola, Buldhana, Jalna, and Parbhani. The state would also have to take up significant efforts to scale up coverage in the district of Pune which is the only district where coverage rates have declined between 2017-18 and 2019-20.
Key Takeaways & Policy Implications
The data showcases the low coverage of a single dose of albendazole tablet post the first trimester in the state. Despite the ease to deliver a single dose of Albendazole tablet preferably during the 2nd trimester (deworming guidelines), the coverage of this intervention is much lower than other ANC services like the distribution of iron and folic acid tablets for a minimum of 180 days from the 2nd trimester and distribution of 360 calcium tablets during the 14th to 40th week of pregnancy.9,11 However, the data also indicates that districts with high maternal anemia gave due importance to the implementation of the deworming intervention. There is hence a need to sensitize health workers in all districts on the importance of deworming to improve maternal health including prevention of anemia.
Information on district-level deworming coverage is vital to improving service delivery. Sensitization of healthcare workers would be critical to scale up coverage in districts with the lowest deworming rates (Pune, Jalna, Buldhana, Akola and Parbhani).
While the coverage gap is highlighted, the severity of this gap at the district level cannot be understood without the availability of district-level STH infection prevalence estimates. The national guidelines on antenatal deworming prescribe universal coverage of pregnant women in STH endemic areas (areas >20% prevalence)7. Understanding the prevalence of soil-transmitted helminth infections at the district level is necessary to plan control strategies and focus on highly endemic regions for preventive therapy as per norms.
Policy Recommendations
Maternal anaemia rates are high at both national and state levels as per NFHS-512. However, HMIS data shows that despite the government’s recognition of the importance of deworming in the reduction of maternal anemia, the evident gap between deworming and other ANC services like IFA distribution indicates that frontline healthcare workers may not perceive its importance. Currently, guidelines require ANMs and medical officers to be trained to ensure knowledge of the program, deworming drugs, their dosage, and administration during the ANC period whereas ASHAs receive an orientation on the program and to support monitoring and counselling for this service.7 Refresher training should also be periodically conducted to reiterate the importance of this intervention.
Healthcare workers need to increase awareness about the importance of deworming among pregnant women, families, and the community. Healthcare workers should be given adequate IEC material and job aids to support community and mother education. Ensuring compliance with the minimum of 4 ANC visits and distribution of mother-child protection cards that help monitor the consumption of albendazole tablets could also help increase the uptake of antenatal deworming.
Currently, the incentive structure of ASHAs, the frontline workers that operate at the community level does not appear to support monitoring the consumption of deworming by pregnant women, unlike IFA consumption13. An incentive for ASHAs to monitor deworming consumption during the ANC period would ensure its better uptake.
References
- Zegeye, B., Keetile, M., Ahinkorah, B. O., Ameyaw, E. K., Seidu, A. A., & Yaya, S. (2021). Utilization of deworming medication and its associated factors among pregnant married women in 26 sub-Saharan African countries: a multi-country analysis. Tropical Medicine and Health, 49(1), 1-15.
- Gyorkos, T. W., & St-Denis, K. (2019). Systematic review of exposure to albendazole or mebendazole during pregnancy and effects on maternal and child outcomes, with particular reference to exposure in the first trimester. International journal for parasitology, 49(7), 541-554.
- Salam, N., & Azam, S. (2017). Prevalence and distribution of soil-transmitted helminth infections in India. BMC Public Health, 17(1), 1-12.
- Walia, B., Kmush, B. L., Lane, S. D., Endy, T., Montresor, A., & Larsen, D. A. (2021). Routine deworming during antenatal care decreases risk of neonatal mortality and low birthweight: a retrospective cohort of survey data. PLoS neglected tropical diseases, 15(4), e0009282.
- Traore, S. S., Bo, Y., Kou, G., & Lyu, Q. (2023). Iron supplementation and deworming during pregnancy reduces the risk of anemia and stunting in infants less than 2 years of age: a study from Sub-Saharan Africa. BMC Pregnancy and Childbirth, 23(1), 63.
- World Health Organization. (2017). Guideline: preventive chemotherapy to control soil-transmitted helminth infections in at-risk population groups. World Health Organization.
- MoHFW. (2014). National Guidelines for Deworming in Pregnancy. Ministry of Health & Family Welfare (MoHFW). Government of India.
- MoHFW. (2010). Guidelines for Antenatal Care and Skilled Attendance at Birth by ANMs/LHVs/SNs. Ministry of Health & Family Welfare (MoHFW). Government of India.
- MoHFW. (2014). National Guidelines for Calcium Supplementation During Pregnancy and Lactation. Maternal Health Division. Ministry of Health & Family Welfare (MoHFW). Government of India.
- MoHFW. (n.d.). Anaemia in 15-49 year old women, Maharashtra, NFHS5 2019-2021. Health Nutrition India. Retrieved from: https://healthnutritionindia.in/dashboard/2/1/71
- NHM. (n.d.) Anaemia Mukt Bharat 6 interventions. National Health Mission. Retrieved from: https://anemiamuktbharat.info/interventions/
- MoHFW. (n.d.). Anaemia in pregnant women, India, NFHS5 2019-2021. Health Nutrition India. Retrieved from: https://healthnutritionindia.in/dashboard/3/1/239
- NHM (n.d.). ASHA incentives – FY 2020-21. National Health Mission
We acknowledge the support of the National Health Mission, CTARA-IIT Bombay, and the GISE Hub, IIT Bombay.
Authors
Marian Abraham, Prof. Sarthak Gaurav
Marian Abraham is a Senior Research Analyst at the Koita Centre For Digital Health, IIT Bombay.
Prof. Sarthak Gaurav is an Associate Professor at Shailesh J. Mehta School of Management, IIT Bombay.
